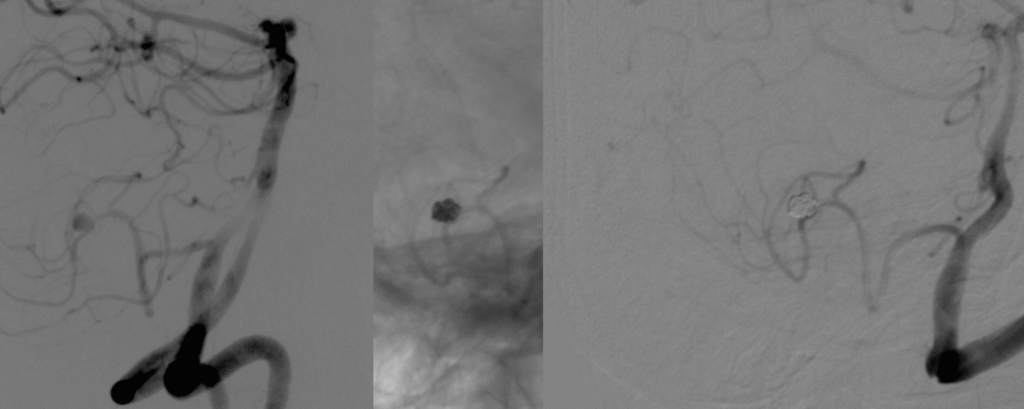
Cerebral Aneurysm Coiling, also known as endovascular embolization, is a minimally invasive technique used to treat brain aneurysms (weak, balloon-like bulges in the wall of a blood vessel).
The primary goal is to seal off the aneurysm from the normal blood circulation, thereby preventing it from rupturing or re-rupturing, which can cause a catastrophic hemorrhagic stroke (bleeding in the brain).
Key Benefits of Cerebral Coiling
Coiling is often the preferred treatment method for many aneurysms due to its less invasive nature compared to traditional open brain surgery (surgical clipping).
| Benefit | Description |
|---|---|
| Minimally Invasive | Requires only a small puncture site (usually in the groin), avoiding the need for a craniotomy (open brain surgery). This leads to less pain and minimal scarring. |
| Reduced Recovery Time | Patients typically experience a significantly shorter hospital stay and faster return to normal activities (often a few days) compared to surgical clipping (which usually takes weeks). |
| Lower Initial Morbidity/Mortality | Studies, such as the International Subarachnoid Aneurysm Trial (ISAT), show that for suitable ruptured aneurysms, coiling is associated with lower rates of death and severe disability at 1 year compared to clipping. |
| Treats Complex Aneurysms | Coiling can often access and treat aneurysms located in deep or difficult-to-reach areas of the brain, particularly in the back (posterior circulation), which are highly challenging for open surgery. |
Understanding the Risks and Potential Complications
While coiling is minimally invasive, it is a complex procedure involving blood vessels in the brain and carries specific risks. Your neurosurgical team will assess your individual risk based on the aneurysm size, location, and whether it has already ruptured.
| Complication Type | Incidence (Likelihood) | Details |
|---|---|---|
| Thromboembolic Event (Stroke/Mini-stroke) | Common (Approx. 3%−15% per procedure) | A blood clot forms on the catheter or coils and travels into the brain, blocking a blood vessel. This is the most common major complication and can cause temporary or permanent neurological deficits. |
| Aneurysm Rupture during Coiling | Low (Approx. 1%−5% per procedure) | The microcatheter, guidewire, or coils may inadvertently puncture the delicate aneurysm sac, causing immediate bleeding. The morbidity and mortality risk for this event is high. |
| Coil Protrusion/Migration | Uncommon (Approx. 0.5%−3% per procedure) | The coils may protrude into the main artery or migrate away from the aneurysm site. This can lead to a stroke or require immediate correction with a stent or balloon. |
| Aneurysm Recurrence (Reopening) | Moderate (Approx. 20%−30% over time) | Over time, the coils may compress or the blood clot may shrink, allowing blood flow back into the aneurysm. This requires lifelong follow-up imaging and may necessitate further treatment (retreatment). |
| Access Site Complications | Common | Bruising, hematoma (swelling/bleeding), or nerve damage at the femoral artery puncture site in the groin. These are usually minor and temporary. |
| In-Hospital Mortality Rate | Very Low (Approx. 0.5%−1.8% for unruptured aneurysms) | The risk of death directly related to the procedure for unruptured aneurysms is very low in high-volume centers. This rate is higher for ruptured aneurysms. |
Sources:
- Molyneux, A., et al. (2002). “International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of outcome at 1 year.” The Lancet.
- Johns Hopkins Medicine. “Endovascular Coiling: Risks and Benefits.”
- UC San Francisco. (2006). “Results of clipping and coiling of aneurysms are similar over time.”
- Neurosurgeons of New Jersey. “Aneurysm Coiling Procedure Risks: What Are They?”
